This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I would like to thank Dr. Vamshi sir and Dr. Kranthi ma'am for providing me the case details.
Case History :
A 38 year old male patient presented to the casualty in a drowsy state on 3th June, 2021 at 10:20 am with
Chief Complaints (c/o) :
1. Weakness of Right upper limb and right lower limb since 2 hours
2. Deviation of mouth towards Left since 2 hours
History of Present Illness :
Patient was apparently asymptomatic 1 month back. Then he presented to OPD for c/o of fever (low grade, not associated with chills and rigor), cold and cough and has been tested positive for COVID-19 and followed protocols of home isolation and was on symptomatic treatment for COVID and after 14 days tested negative for COVID-19.
No history of Shortness of breath, Orthopnea, Paroxysmal Nocturnal Dysuria.
No history of palpitations, chest pain, syncopal attack.
Patient suddenly developed weakness of Right upper limb and Right lower limb on 3rd June, followed by deviation of mouth to left during having food at 10:00 am.
History of weakness of bilateral lower limbs since 3-4 days.
History of pedal edema (Grade 2) and there is no diurnal variation
No history of headache, nausea, vomiting, loose stools.
No history of tingling sensation, numbness.
No history of involuntary micturition, defaecation.
Past History :
Patient is a known case of Hypertension since 6 months and is not on medication.
Patient is not a known case of Diabetes mellitus, Epilepsy, Coronary Artery Disease, Tuberculosis, Asthma.
Personal History :
Appetite - Normal
Diet - Mixed
Bowel movements - Regular
Micturition - Normal
Addictions - Consumes alcohol regularly
Family History :
There is no significant family history.
General Examination :
The examination was done after obtaining informed consent in a well lit room.
Patient was drowsy and arousable, aphasic and was not oriented to time, place and person.
There was no pallor, icterus, cyanosis, clubbing and lymphadenopathy.
Bilateral pedal edema was present (since 3-4 days)
Vitals :
At the time of admission :
Temperature : 98.4o F
Pulse Rate : 92 bpm
Blood Pressure : 160/110 mm Hg
Respiratory Rate : 22 cycles /min
SpO2 : 98% on Room air
GRBS : 106 mg%
Systemic Examination :
Respiratory System : BAE +
Cardiovascular System : S1,S2 heard
Per Abdomen : Soft, non-tender
CNS : Weakness of Right upper and lower limb
Patient is in altered sensorium
GCS : E4V1M5
- 10
• On the day of admission (3-6-2021) :
Reflexes : Absent
Plantars : mute
Tone : Hypotonia on right side
Normal on left side
Power : Right upper limb & lower limb flickering movements
Left upper limb & lower limb moving spontaneously but grade can't be assessed as the patient is in altered sensorium.
• Next day (4-6-2021) :
Similar Findings except
Reflexes - Right side : Absent
Plantar(mute)
- Left side : +2
Plantar(withdrawal)
Investigations :
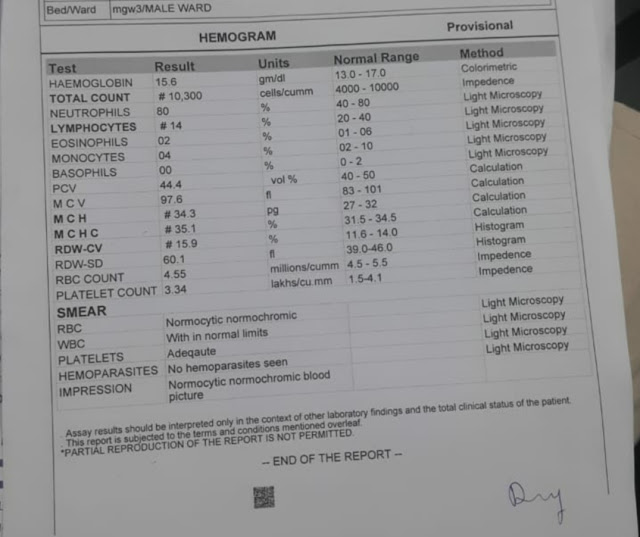
Hemogram :
Serum Electrolytes :
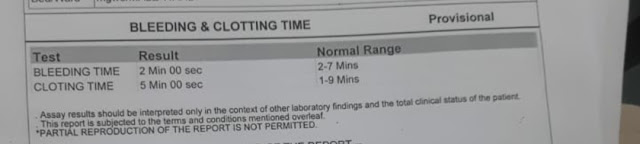
Bleeding & Clotting Time :
Fasting Blood Sugar :
Fasting Lipid Profile :
Renal Function Tests :
Urea : 15 mg/dl
Creatinine : 0.8 mg/dl
Uric acid : 6.1 mg/dl
Ca+ : 10.2 mg/dl
PO4-3 : 3.1 mg/dl
Na+ : 135 mg/dl
K+ : 3.1 mg/dl
Cl- : 103 mg/dl
Liver Function Tests :
AST : 23 units/lit
ALT : 22 units/lit
ALP : 375 units/lit
Total Bilirubin : 1.14 mg/dl
Direct Bilirubin : 0.20 mg/dl
A/G Ratio : 1.39
MRI Brain :
Ultrasound Scan :
ECG :
Colour Doppler 2D ECHO :
Diagnosis :
Acute Ischemic Stroke with infarcts in Caudate and Putamen, left IC, Left Insular cortex, Left fronto-parietal and temporal lobes.
Treatment :
1. Tab Ecospirin - 150 mg PO/OD
2. Tab. Clopitab - 75 mg PO/OD
3. Tab. Atorvas - 40 mg PO/OD
4. Inj. Optineuron - 1 ampoule 100ml/NS/IV BD
5. Inj. Mannitol 100 ml IV/TID
6. BP/PR/RR/Temp monitoring 6th hourly
7. Physiotherapy - Right upper limb and lower limb
8. IVF - 2O NS @75 ml/hr
9. Inj Thiamine i amp in 100 ml NS/IV/TID










Comments
Post a Comment